College Students' Perspectives Regarding Fertility Preservation
Pierre, Dudith
University of South Florida Tampa, Florida, USA
Abstract
-The purpose of this research is to examine college students' attitudes and knowledge of fertility preservation for cancer patients. The specific hypotheses were that students would have low levels of knowledge about the effects of chemotherapy on fertility and that religion would play a key role in their decision to accept fertility preservation if they had a cancer diagnosis. - A sample of 239 students from upper-level classes at the University of South Florida was surveyed in order to assess knowledge and attitudes of college students. The survey consisted of questions derived from a survey administered at the 2007, “Facing Our Risk of Cancer Empowered” (FORCE) conference, and additional specific questions regarding cancer and fertility preservation aimed at general audience. -In the case of a cancer diagnosis, 77.4% of students disagreed that religion would play the most important role, in their decision to accept fertility preservation. Most students (43.5%) agree that their partner would play a more important role than religion. In their decision to accept or reject fertility preservation, and 33.1% of them strongly agreed high percentage of the students (75.3%) knew that chemotherapy caused sterility. -The data reinforce that patients from all educational level from all religious and ethnic backgrounds should be informed about the damages chemotherapy can cause and the fertility preservation options available to them depending on their age and gender
Citation
College Students' Perspectives Regarding Fertility Preservation. Pierre, Dudith . Lethbridge Undergraduate Research Journal. Volume 4 Number 2. 2009.
Introduction
At any age, a cancer diagnosis is devastating. It is devastating not only to the patient, but also to the patient's family members and friends. Chemotherapy offers hope, especially when the cancer is detected early. Because chemotherapy offers hope, the number of cancer survivors in all age groups is augmenting. Fertility preservation is of importance only to the patients in or below the reproductive age. When any patient is diagnosed with cancer, the greatest concern is survival, but for patients in reproductive age, the ability to become a biological parent is a secondary concern. It is not always considered so at the time of diagnosis and treatment, but after a successful treatment, it becomes very much so.
Many patients diagnosed in their reproductive age manifest the desire to become biological parents after their treatment. However, many of them were not offered fertility preservation options before they went through chemotherapy. The number of young cancer survivors is increasing; therefore, the problem becomes more pronounced. As the cancer survivors see their treatment in retrospect, they remember that their oncologist did not inform them of the effects of chemotherapy on their reproductive system and about the fertility preservation options available to them.
This research examines college students' attitudes and knowledge regarding fertility preservation for cancer patients. The primary hypotheses were that students would have low levels of awareness about the effects of chemotherapy on fertility and that a students' religion would play the most important role in his or her choice to accept or reject fertility preservation. The secondary hypotheses were that having a relative with cancer or speaking English as a primary language would impact knowledge and attitude regarding fertility preservation.
Literature Review
Chemotherapy can affect fertility, but cancer itself can have a negative impact on fertility. Abnormal sperms and reduced sperm production have been found in men with untreated Hodgkin lymphoma and testicular cancer (Shin, Lo, & Lipshultz, 2005). Damage of the reproductive system leading to infertility in both gender is caused by several factors such as the type of drug and the dosage, the patients' reproductive status, the radiation location and dosage, the patients' pubertal status and the patients' pre-treatment fertility (Bahadur et al., 2006).
Effects of chemotherapy on men
The main injuries caused by chemotherapy in men are reduction of sperm production, poor sperm quality and motility, and DNA damage, which can be caused by either chemotherapy or radiation. Infertility caused by Chemotherapy can be temporary or permanent. Because chemotherapy has an effect on cells that are dividing uncontrollably, it can cause a lack of development in the germinal cells located in the seminiferous tubules; this may lead to reduced sperm production. When treatment is completed, male gonads take time to recover their function. The probability that they will recover their function depends on the male's age and the dosage of the chemotherapeutic agent. The time it takes for spermatogenesis to resume its function in some men seems to be dependent on the dosage level. The treatment agents used in combination appear to have an increased impact on fertility (Bahadur et al., 2006).
Effects of chemotherapy on women
Unlike in men, chemotherapy can damage many reproductive organs in women; these organs include the cervix, the uterus, the fallopian tubes and the ovaries. However, cancer, by itself, does not negatively impact women's fertility. While chemotherapy itself can affect these organs, their surgical removal due to can will certainly lead to infertility (Bahadur et al., 2006). Menopause resulting from chemotherapy may be caused by direct injury to the ovaries or indirect injury causing detriment of follicular cells. chemotherapy can also accelerate menopause (Lee et al., 2006). Chemotherapy can cause immediate sterility and premature menopause in women; it can damage the uterus and cervix, leading to inability to become pregnant or carry a baby (Bahadur et al., 2006). Temporary or permanent premature ovarian failure can result from chemotherapy. Chemotherapy can also cause ovarian fibrosis, which leads to failure of ovulation, absence of periods or irregular periods, and ultimately infertility. Age plays an important role in the effects chemotherapy has on the ovaries. Younger women's ovaries tend to be less affected than those of older women. The probability that the menstruation will resume depends on the drug, the dosage, and the woman's age. The probability that menstruation will return in women younger than 40 years of age is greater than that of women older than 40 years of age. When a combination of drug is used, there is less chance that menstruation will resume (Lee et al., 2006).
Fertility preservation options for men
Many fertility preservation options are available to men; the option chosen depends on the man's age. Some options that may be ideal for men before puberty may not be so for men after puberty. Sperm banking is one of the most reliable fertility preservation options. Sperms are assessed, frozen and stored. This option is ideal for men after puberty. Another option is testicular tissue freezing, which is the surgical removal of the stem cells that produce sperms. The tissue is evaluated, frozen, and stored. This option is practical for men after puberty. Both sperm banking and testicular tissue freezing are practical options before chemotherapy. Testicular sperm extraction is practical for patients who are not producing sperm after treatment. The testicular tissue is removed and analyzed for remaining sperm cells. Any sperm found is used for in vitro fertilization (Singh, Davies, & Chatterjee, 2005). Radiation shielding of gonads is an option that can be used by men both before and after puberty. The gonads are shielded during treatment to reduce the radiation dosage to the testes (Bahadur et al., 2006). Other options are available for survivors that cannot be biological parents; these options are donor sperm, donor embryos, and adoption (Singh et al., 2005).
Fertility preservation options for women
There are even more fertility preservation options for women than men. Egg freezing is an ideal option for women before and after treatment. Eggs are removed, frozen, and stored. Ovarian tissue freezing is an option available to women before and after treatment. Ovaries are removed, frozen, and then transplanted after the treatment. In ovarian transposition, the ovaries are surgically transposed to reduce their exposure and damage that can result from chemotherapy and radiation. They must be transposed before treatment. Radical trachelectomy is an option used mainly by cervical cancer patients. It is the surgical removal of the cervix and the preservation of the uterus. During treatment, ovarian suppression by gonadotropin-releasing hormones (GnRH) is another way of protecting the ovaries from damages that can result from chemotherapy and radiation. One of the most successful options is embryo freezing. Eggs are fertilized outside of the body and frozen (Sing et al., 2005). Radiation shielding of gonads is also available to women. Reproductive organs are shielded from exposure and damage of chemotherapy and radiation. Donor eggs, donor embryos, gestational surrogacy, and adoption are other options that survivors can consider (Bahadur et al., 2006).
Complications in Pregnancy
Despite the increasing number of fertility preservation options available to cancer patients before and after treatment, there is no guarantee that the patient will become a biological parent. The probability of getting pregnant is not 1 (one) in any of the options. Even if pregnancy results, the chance of complications is high. In cancer survivors, there is a greater probability of low birth weight, premature infants and miscarriages. Depending on the type of cancer the survivor suffered from, there is risk of cardiac and pulmonary insufficiency during pregnancy. The cardiac and pulmonary insufficiency can also be caused by the stress resulting from the pregnancy (Quinn et al., 2008).
Method
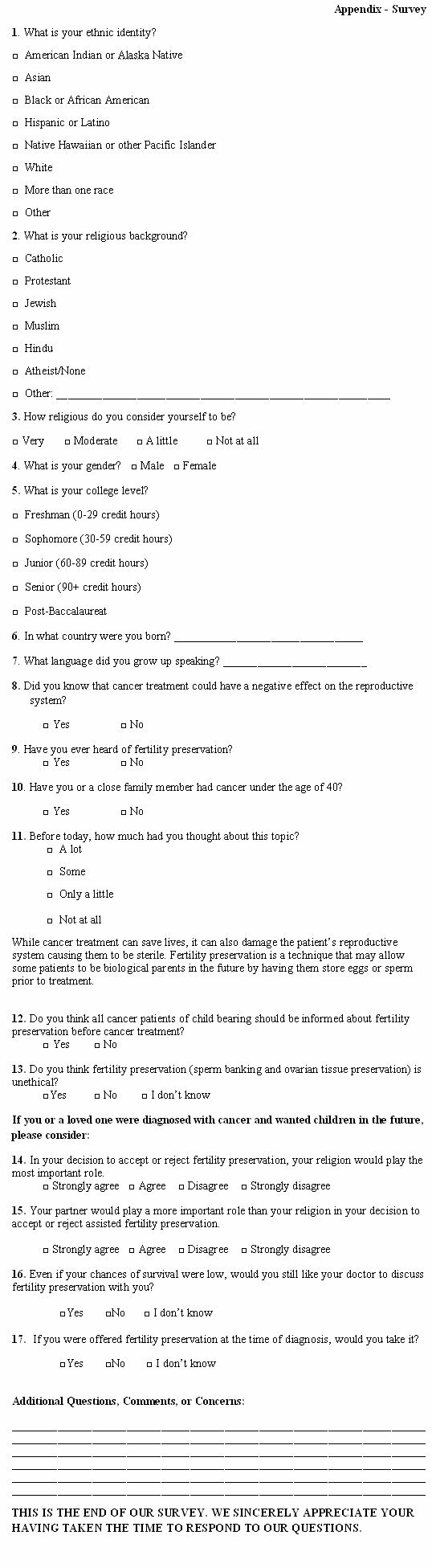
A sample of 239 students from upper-level classes at the University of South Florida was surveyed in order to assess their knowledge and attitudes of college students. The classes surveyed were in the department of biology, social work, psychology and public health. The majority of the students found in those classes were juniors and seniors. The survey was composed of 17 questions (See appendix) and was anonymous. The questions were of three types: demography, knowledge and attitude. The survey took about 10 minutes to be completed. The surveys were scanned, and the percentages were computed. The survey was totally optional; the students did not have to meet any requirements to take to survey. All completed questionnaires were read by an optical scanner using Teleform (Verity Software), a high-accuracy content capture system for automatically processing paper-based forms. If a response (s) could not be read by Teleform, data were manually entered. The survey consisted of question from a survey administered at the 2007 “Facing Our Risk of Cancer Empowered” (FORCE) conference, including new specific questions regarding cancer and fertility preservation.
Results
A sample of 239 students was surveyed concerning knowledge and attitude of fertility preservation. The sample presented a combination of 45.2% Caucasian, 15.9% Blacks, 14.6% Hispanics, 12.7 % Asians, and 12.6% students of other races including multiracial individuals (Table 1). More than half of the 239 students were seniors, 31.8% juniors and 13.8% freshmen and sophomores. Of the 239 students, females made up the largest percentage (62.3%), and 90 (37.7%) were males (Table 1).
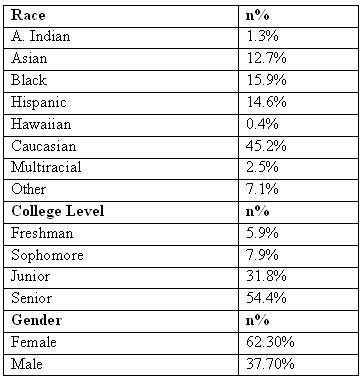
Table 1: Standard Demographics
The majority of the students surveyed were born in the U.S. (78.2%), and the majority of them considered English their primary language (71.5%). Most of the participants did not have a relative less than 40 years of age affected with any type of cancer (Table 2).
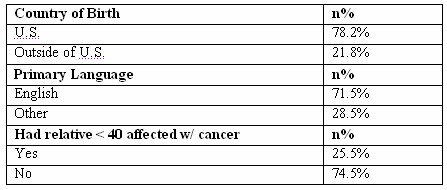
Table 2: Demographics
Of the 239 students, the largest religious group was Catholic (25.9%), and the second largest was Protestant, which made up 15.9% of the participants. Jewish, Muslim and Hindu religions made up 13%, with 8.8% reporting they had no religious affiliation, and the remaining 36% reported not being affiliated with any of the religions mentioned above. The majority of the students surveyed reported that they were moderately religious (43.5%). The second largest group reported that they were only a little religious, while only 13% of participants were very religious and 15.5% were not religious at all (table3).
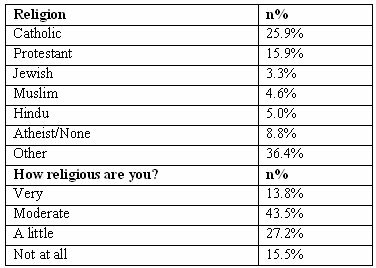
Table 3: Religion
A very high percentage of students (96.2 %) agreed that patients in reproductive age should be informed about fertility preservation before cancer treatment. Many students thought that fertility preservation is ethical (83.7%). Some students reported that they did not have any knowledge whether it was or was not ethical and only 2.5% believed that it was unethical. In the case of a cancer diagnosis, in their decision to accept fertility preservation, 77.4% of students disagreed that religion would play the most important role (table 4). Most students (43.5%) agreed that their partner would play a more important role than religion in their decision to accept or reject fertility preservation; 33.1% of them strongly agreed. Only 7.5% of the students strongly disagreed, and 15.9% of them disagreed. Many students (79.1%) wanted to be offered fertility preservation even if their chance of survival was low, while 9.2% said no and 12.6 % did not know. If offered fertility preservation, 49.8 % of the students would accept it, 7.5 % would reject it, and 42.7% did not know what their decision would be.
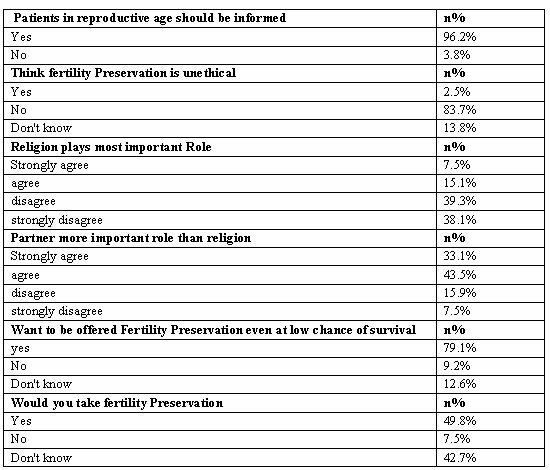
Table 4: Attitude towards Fertility Preservation
A high percentage of the students (75.3%) knew that chemotherapy caused sterility; however, only 48.1% of them have never heard of fertility preservation (table 5). The largest group of students gave the topic some thought (33.1%) and the second largest group (27.6%) thought about the topic only a little. Only 14.6% thought a lot about it, with the remaining 24.7% of them not thinking about it at all.
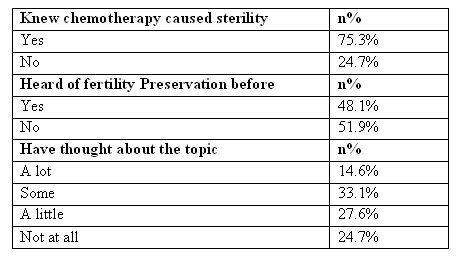
Table 5: Knowledge of Fertility Preservation
Discussion
My primary hypotheses were that religion played the most important role in a person's choice to accept or reject fertility preservation and about half college students do not know that cancer treatment affects the reproductive system in a negative way. The data did not support my first hypothesis because only 22.6% of the participants agreed that religion would play the most important role in their decision to accept or reject fertility preservation. Instead, 73.6% of them reported that their partner would play a more important role than their religion when making such a decision. Even among the students who claimed to be very religious, 51% of them disagreed that religion would play the most important role in making that decision, and 67% of those who claimed to be moderately religious also disagreed.
I also hypothesized that about 50% of college students did not know that chemotherapy had negative effects on the reproductive system. This hypothesis was not supported by the data; only half on the value hypothesized (24.7%) did not know. One factor that explains this low percentage is that 86.2% of the participants were upper-level students. Also, if the question was a true of false one, the percentage could be higher (see question 8 in appendix). Students born in the U.S. made up 69% of those who did not know that chemotherapy negatively affected the reproductive system, and the remaining 31% were born outside of the U.S. Of the students who were born in the U.S. and did not know, 10% of them did not speak English as their primary language. Being born in the U.S. did not increase the students' chance of knowing that chemotherapy had negative effects on the reproductive system.
Students who did not have family members younger than 40 years of age affected with cancer still thought about the topic (refer to question 10 &11 of survey in appendix). Surprisingly, 35% of the 178 who did not have an affected family member younger than 40 years of age never thought about the topic compared to 15% of those who had affected family members never thought about the topic. In addition, 18% of those with affected family members thought a lot about the topic while 12% of those without such a family member did so. It seems that students with affected family member younger than 40 years tend to think and spend more time thinking about the topic than those without such family members.
The data revealed that 51.9% of the students never heard of fertility preservation. This is very surprising considering that half of the students were seniors. The majority of them knew that chemotherapy could damage the reproductive system; however they did not know that the fertility of the cancer patients could be preserved. Moreover, 96.2% of them agreed that cancer patients in their reproductive age should be informed about the effects of chemotherapy on the reproductive system. Even with a low chance of survival, 79.1% of them wanted to be informed about fertility preservation. Their attitude about accepting fertility preservation was somewhat scattered. While 51.9% of them never heard of fertility preservation, 49% of those 51.9% reported that they would accept fertility preservation if they were diagnosed with cancer. Of the 239 participants, 49.8% of them reported that they would accept fertility preservation, 7.5% would not, and 42.7% were undecided.
Conclusion
Contrary to the first hypothesis, partner replaces religion in deciding whether or not to accept fertility preservation. Certainly, this cannot be assumed for the older generation, but it can be expected. Oncologist cannot assume, based on religion, that a patient will not accept fertility preservation. Also, a patient's college level cannot indicate if the patient knows that chemotherapy negatively affects the reproductive system to the point of causing sterility because the students who did not know were found in upper and lower level classes. About one-quarter of the students surveyed did not know about the effects of chemotherapy on the reproductive system; it can certainly be argued that it is not a very large number. However, it can be inferred from this information that the number becomes larger as educational level decreases. This number would become even larger if such a survey was given to people with a substantially low educational level and English proficiency. Despite the fact that the data did not support my hypotheses, it revealed that about half of the students did not know the fertility of a cancer patient could be preserved. When such a high percentage of college students never heard of fertility preservation, it probes one to ask what percentage of the general population has heard about fertility preservation, while taking into account Americans who did not complete high school, and those from minority groups whose English proficiency is very low.
The data reinforce that individuals from all educational levels, religious and ethnic backgrounds should be informed about the damages chemotherapy can cause and the fertility preservation options available to them depending on their age and gender. In addition, brochures can be made for minority patients in their primary language to ensure that they know about fertility preservation options available to them and the risks involved in cancer treatment. It is very important that the patient's partner is present during the information session between the oncologist and the patient since the partner, for most patients, will play the most important role in deciding to accept or reject fertility preservation. I hope this article encourages researchers to further explore this issue by interviewing cancer survivors.
Acknowledgements
I would like to thank Dr. Quinn for her patience and instructions. I would also like thank Michelle Griffith, Lindsey, Naomi and Dr. Maher for all their support throughout this project.
About the Author
Dudith Pierre transferred from Palm Beach Community College to attend University of South Florida in August 2006; she received her bachelors degree from University of South Florida in May 2008. Her hobbies are poetry writing, reading, and community service. She plans to attend Florida International University to obtain a graduate degree in public health.
References
Shin, D., Lo, K. C., & Lipshultz L. I. (2005). Treatment Options for the Infertile Male With Cancer. Journal of the National Cancer Institute Monographs, 48-50.
Bahadur, G., Ling, K.L.E., Hart, R., Ralph D., Wafa R., Ashraf A., Jaman, N., Mahmud S., & Oyede A.W. (2006). Semen quality and cryopreservation in adolescent cancer patients. Human Reproduction, 17, 3157-3161.
Lee, S. J., Schover, L. R., Partridge, A. H., Patrizio, P., Wallace, W. H., Hagerty, K., Beck, L. N., Brennan, L. V., Oktay, K. (2006). American Society of Clinical Oncology Recommendations on Fertility Preservation in Cancer Patients. Journal of Clinical Oncology, 24, 2917-2931
Singh K. L., Davies, M., & Chatterjee R. (2005). Fertility in Female Cancer Survivors: Pathophysiology, Preservation and the Role of Ovarian Reserve Testing. Human Reproduction Update, 11, 69-89.
Quinn G.P., Vadaparampil S. T., Bell-Ellison B.A., Gwede C.K., Albrecht T.L. (2008). Patient-Physician Communication Barriers Regarding Fertility Preservation among Newly Diagnosed Cancer Patients. Social Science and Medicine, 66, 784-789.